Women over 40 now account for almost one in five IVF procedures in the UK, according to new figures. 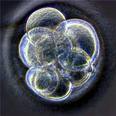
The figures, published by the Human Fertilisation and Embryology Authority (HFEA), which regulates the fertility industry in Britain, show that proportion has almost doubled in the last 13 years.
In 1998 the over 40s only accounted for 10 per cent of IVF cycles, according to the HFEA, but last year they accounted for nineteen per cent of IVF cycles.
Figures compiled by the authority showed 13.6 per cent of IVF cycles in 2010 were in 40 to 42-year-olds; 3.5 per cent in 43 to 44-year-olds, and 1.9 per cent in those aged 45 or over.
The average age of women having IVF has also risen by 18 months since 1991, from 33.6 years to 35.1 years.
Studies are increasingly showing that older women are making up a higher proportion of clients at more and more fertility clinics.
The Harley Street Fertility Clinic this week said around 40 per cent of those attending were over 40, while the Lister Hospital in London reported almost a third were.
Dr Marie Wren, deputy medical director at the Lister, said: “If you look at the older women we have treated in the last three years, the number has risen significantly. I think part of the reason is that women are now aware that it is possible to try to get pregnant at an older age.
“Increasingly, an awful lot of 40-plus women don’t see themselves as old. Many are fit and healthy and look extremely youthful.”
Almost all those over 40 undergoing IVF are likely to be private patients at the moment, as guidelines from the National Institite of Health and Clinical Excellence (Nice) currently limits NHS provision of IVF to women aged 23 to 39.
However, that stipulation could soon be relaxed as the guidance, written in 2004, is due to be updated.
The total number of IVF cycles has also been rising rapidly, by 5.9 per cent between 2009 and 2010 alone, found the HFEA.
That is against a backdrop of increasingly limited NHS provision, with cash-strapped health authorities cutting back by tightening qualifying criteria.
The number of pregnancies resulting from IVF or intra-cytoplasmic sperm injection (ICSI), a technique used to combat male-factor infertility, grew from 12,386 to 13,015 – a 5.1 per cent increase.
The NHS paid for a slightly higher proportion of IVF cycles last year than in 2009.
Most cycles are still paid for privately, but the proportion funded by the NHS grew from 38.5 to 40.6 per cent between 2009 and 2010.
Meanwhile, here, a leading neonatologist has said that more babies are being born prematurely because of the rising age of mothers and increased use of in-vitro fertilisation treatment, among other factors.
Dr John F Murphy, clinical lead of the Health Service Executive’s neonatology programme, was speaking at the launch of a report by a charity calling for development of a national neonatal health policy, according to the Irish Times.
“The Irish prematurity rate of 6 per cent is rising steadily due to a series of factors including increased maternal age, IVF treatment, multiple births, obesity and other dietary factors and the catch-all effect of greater urbanisation,” he said.
The older age of mothers resulted in more hypertension affecting the nutrition and blood flow to the infant and meant doctors had to intervene early, Dr Murphy said.
The rise in IVF led to more twinning, which increased prematurity. General increased urbanisation and nutrition were also factors. The increase in the birth rate was another factor in the rise in premature births, Dr Murphy added. Irish birth rates rose 40 per cent between 1999 and 2009.
The increase in overall births “happened quite quickly” and “caught us all out, as it’s hard to legislate for”, he said.
Many infants whose birth weight and gestation period fell outside the remit for automatic follow-up were failed by aftercare, the report added. Potential high- risk developmental issues became the responsibility of the family or GP, it said.















